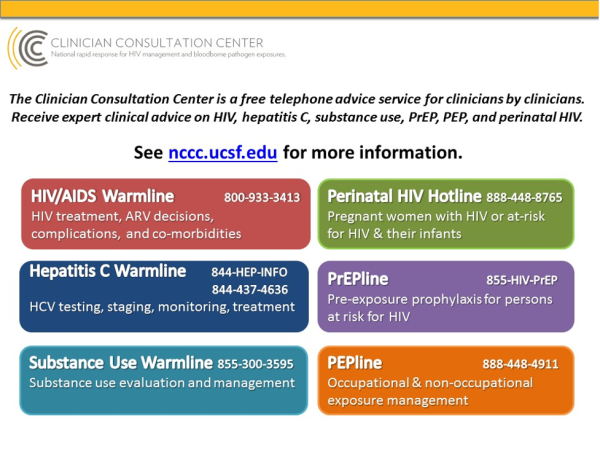
Pharmacists have been identified by the CDC as key professionals in achieving one of the CDC’s goals of Ending the HIV Epidemic in the U.S. by preventing HIV infection. Below are some of the most common questions received at the AETC National Clinician Consultation Center (NCCC) from pharmacists about pre-and post-exposure prophylaxis (PrEP and PEP). Click on each question or statement to expand for answers and recommendations. Visit the NCCC website to see other QAs about using PrEP and PEP effectively. Clinical consults about PrEP/PEP can also be obtained by calling the NCCC at the numbers listed below:
Pharmacists are uniquely positioned to expand PrEP/PEP awareness and increase PrEP/PEP prescribing to prevent HIV infection, especially in populations disproportionately affected by HIV, including Blacks, Latinos, women, and adolescents and young adults. Pharmacies may be more accessible to at risk persons not engaged in health care by providing more convenient locations and more flexible weekend and evening hours. Pharmacists are knowledgeable and trusted health professionals that can provide timely access to oral PrEP/PEP without the need for appointments. Studies show that pharmacist provision of PrEP is well received by patients (Zhao A et al, 2021). Additionally, pharmacies might be an alternative setting to administer IM cabotegravir PrEP if logistics and billing issues are resolved.
Certain states (e.g., California, Colorado, Oregon, Nevada, Washington, Maine, Virginia, New Mexico) have passed legislation that allow pharmacists to independently initiate PrEP/PEP in their pharmacy setting. PrEP/PEP can also be independently provided by pharmacists by constructing a collaborative practice agreement with physicians or their local Public Health Department. Many states are in discussions regarding pharmacists’ prescriptive authority to aid in ending the HIV epidemic.
Knowledgeable and motivated pharmacists can play an important role in HIV prevention and PrEP/PEP awareness by facilitating a conversation about PrEP with interested persons and offering PrEP to sexually active persons and persons who inject drugs (PWIDs). Pharmacists can ask all persons “Do you know about PrEP/PEP and what it does?” PrEP can be provided to any person who asks for PrEP even if no risky disclosure is identified. Disclosure may not be appropriate due to personal reluctance or concerns about stigma. Pharmacists can link persons not engaged in care by providing provider resources.
Pharmacists can provide or reinforce prior education about comprehensive HIV risk reduction strategies, including HIV testing and counseling, sexually transmitted infections (STI) assessment and treatment, clean syringes for PWIDs to prevent HIV/HBV and HCV infections, proper condom use, and U=U (undetectable equals untransmissible) in those with partner(s) with HIV. People with HIV with undetectable HIV viral loads for 6 months or more cannot transmit HIV sexually to their partner(s), and PrEP adds additional HIV protective benefits for partners without HIV.
Pharmacists can be strong advocates for increasing essential immunizations and reducing vaccine hesitancy. Clients accessing PrEP/PEP can obtain recommended vaccines at one-stop pharmacies that offer expanded pharmacy services, including vaccines (e.g., hepatitis A and B, human papillomavirus, influenza, SARS-CoV-2, pneumococcal), smoking cessation aids, emergency contraception (Plan B), naloxone (to reduce overdose fatalities in PWIDs), and STI screening by teaching patients to self-collect relevant specimens for testing.
A common barrier to PrEP/PEP accessibility for many uninsured clients is cost. Pharmacists can help clients pay for PrEP/PEP by enrolling persons in co-pay and manufacturer assistance programs. Generic FTC/TDF is available. Prior authorization is not needed by most insurance companies. PrEP/PEP co-pay assistance is available through the pharmaceutical manufacturers, and there are other programs for uninsured clients.
Federal Ready, Set, PrEP program
Patient Advocate Foundation if <400% of FL
Pan Foundation if <500% of FPL
Daily dosing of FTC/TDF or FTC/TAF PrEP is generally safe and well tolerated. Counseling patients about initial side effects to expect when starting PrEP increases patients’ understanding in their own care and can reduce self-discontinuations due to start-up-side effects.
- Initial start-up symptoms of nausea, headache, flatulence, soft stools, headache, and fatigue are self-limiting and usually resolve within the first few weeks even with continuation.
- Counseling persons to administer oral PrEP/PEP with food may reduce GI intolerance.
- Supportive OTC anti-nausea, anti-diarrheal, and analgesics can be recommended temporarily to improve tolerability but should not be required or continued for the entire treatment duration.
- Toxicities are rare and generally do not require stopping PrEP (<2%).
- Renal dysfunction, bone mineral density (BMD) loss, and metabolic changes differ between FTC/TDF and FTC/TAF and are usually reversible after stopping PrEP.
- Chronic FTC/TDF is associated with eGFR declines of 1-5 ml/min; the clinical importance of this decline is unclear, especially in those with normal baseline renal function, and usually reversible once Ftc/TDF is stopped.
- Acute renal failure and Fanconi’s syndrome are rare.
- Avoid FTC/TDF if estimated creatinine clearance (eCrCl) is < 60cc/min.
- In contrast, FTC/TAF is associated with less renal dysfunction. The Discover trial in men who have sex with men (MSM) and in transgender women reported an eGFR increase of 1.8 ml/min with FTC/TAF versus FTC/TDF. Fanconi’s syndrome was not reported.
- Administer FTC/TAF if eCrCL > 30cc/min or after hemodialysis. Monitoring renal function every 6 months is recommended in those with an increased risk of renal toxicity: >50 years old, baseline eCrCL<90 cc/min, coexisting comorbid conditions (e.g., diabetes, high blood pressure), or frequent high dose NSAIDS use. Otherwise, renal function can be monitored yearly.
- Renal dysfunction can be minimized by avoiding dehydration and chronic high dose NSAIDS use.
Protein supplements can falsely increase serum creatinine and result in inaccurate declines in eCrCl.
- Small declines in BMD loss (≈ 1%) are reported with FTC/TDF versus FTC/TAF. The significance of TDF BMD loss is unclear since atraumatic fractures are not increased, and BMD normalizes even if TDF is continued. Any BMD loss on FTC/TDF is improved when changed to FTC/TAF.
- DXA monitoring is not recommended unless there is baseline osteoporosis/osteopenia or if there are concerns about using FTC/TDF in adolescents before completion of bone formation.
Tobacco cessation, alcohol restriction, exercise, and calcium/vitamin D 400 IU supplements can be recommended to support bone health.
- Metabolic changes have been observed. FTC/TDF can reduce LDL/HDL lipids and weight due to an appetite suppression effect. In contrast, FTC/TAF can increase TG/cholesterol and weight by approximately 1.7 Kg. The impact of these changes on pre-existing cardiovascular and metabolic disorders is unclear. The 2021 PrEP guidelines recommend monitoring lipids at baseline and every 12 months while on FTC/TAF, and starting lipid-lowering agents, if indicated based on ASCVD risk scores.
- Only FTC/TDF is recommended in cisgender women and transgender men as PrEP during preconception. FTC/ TAF is not FDA-approved as PrEP for receptive vaginal sex due to lack of efficacy data although studies are in progress. Minimal levels of FTC/TDF are found in breastmilk.
Effective pharmacist and client communication should acknowledge cultural and gender differences before counseling about PrEP/PEP. The pharmacists should provide a confidential environment to discuss and provide counseling about sensitive issues. Try to ascertain how the client would like to be addressed (he, him, she, her, etc.) and the sexual and gender identity of the client (transgender, cisgender, non-binary, bisexual, gay, same-gender loving, queer, etc.).
Excellent adherence is essential for PrEP efficacy. When used correctly, PrEP can reduce the risk of HIV infection through sexual transmission by 99% and through injection drug use by 74-84%. Strict adherence appears to be more forgiving in cisgender men who have sex with men (MSM) than in cisgender women who have sex with men.
A pharmacokinetic study of MSM administered FTC/TDF observed a relationship between dosing and intracellular HIV protective tenofovir diphosphate concentrations. HIV prevention was estimated to be 99% with daily adherence of 7 doses per week, 96% for 4 doses per week and 76% for 2 doses per week The time to protective FTC/TDF intracellular levels in vaginal tissues occurred after 21 days vs 3 to 7 days in colorectal tissue for men. Physiologically, the lower forgiveness of missed doses in women may be due to tenofovir’s shorter half-life in cervicovaginal tissues compared to colorectal tissue. Protective FTC/TDF drug levels required 6-7 weekly doses (>85% adherence) for vaginal tissues but only 2 doses per week (28% adherence) for colorectal tissue. Also, concentrations of tenofovir are 10-fold higher in rectal tissue compared with cervicovaginal tissues. An initial double dose of FTC/TDF in men may be considered to decrease the time to protective TDF levels; data is not available in women.
For FTC/TDF, 2:1:1 nondaily PrEP dosing (event-driven, on demand, intermittent), although not FDA approved, has been shown to be effective in clinical trials of MSM and transgender women only. This dosing strategy has not been proven effective for FTC/TAF or in women and should be avoided until data becomes available. For 2:1:1 FTC/TDF dosing, 2 tablets are administered at least 2 to 24 hours (preferred) before intercourse and then one tablet is taken again 24 and 48 hours after the initial 2 tablets. Using this dosing approach, >95% of persons achieved effective colorectal tissue concentrations at the time of and for > 240 hours after the exposure.
Therefore, when starting PrEP, it is imperative to counsel and educate patients on the time it takes to achieve adequate HIV protective levels and the need for maintaining excellent adherence. Adherence to PrEP should be reviewed at every PrEP visit. Pharmacy refill histories may be helpful in determining degree of adherence. Educate patients that if PrEP is stopped, HIV protection will wane over 7-10 days so that discussions about alternative methods to protect against HV need to occur.
Same day or telehealth PrEP has been shown to be effective models of PrEP uptake and increased PrEP retention. Here are models of pharmacy telehealth PrEP: State of Iowa and Ohio Equitas Health.
- 2021 PrEP Guidelines
- Liverpool HIV drug interaction website
- CDC How to take a sexual history using the 5P’s
- Applying for a CLIA certificate for HIV Testing
- Virtual instructor led PrEP Trainings
- Designing a collaborative practice protocol to allow pharmacists to furnish PrEP/PEP
- Collaborative Practice Agreements and Pharmacists’ Patient Care Services
- Collaborative Practice Agreements: Explaining the Basics
What to do about patients who have difficulty or aversity to swallowing PrEP/PEP pills. Liquids are available usually as pediatric formulation but usually the amount of liquid is large. Solubility about PrEP/PEP regimens are available at University of Toronto Immunodeficiency Clinic.
CDC US Public Health Service. Pre-Exposure Prophylaxis for the prevention of HIV Infection in the United Sates—2021 Update. A Clinical Practice Guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
Castillo-Mancilla JR, Zheng J-H, Rower JE, et al. Tenofovir, emtricitabine, and tenofovir diphosphate in dried blood spots for determining recent and cumulative drug exposure. AIDS research and human retroviruses. 2013;29(2):384-390).
Cottrell ML, Yang KH, Prince HMA et al. A translational pharmacology approach to predicting outcomes of PrEP against HIV in men and women using TDF with or without FTC. J. Infect Dis 2016;214 (1):55-64)
Havens JP, Scarsi K, Sayles H, et al. Acceptability and Feasibility of a Pharmacist-Led Human Immunodeficiency Virus Pre-Exposure Prophylaxis Program in the Midwestern United States, Open Forum Infectious Diseases, Volume 6, Issue 10, October 2019, ofz365, https://doi.org/10.1093/ofid/ofz365
Hocqueloux L, Lefeuvre S, Bois J, Valentin C, Brucato S, et al. Bioavailability of solid vs. dissolved vs. crushed single-tablet of bictegravir/emtricitabine/tenofovir alafenamide in HIV negative volunteers: the SOLUBIC study. 18th European AIDS conference (EACS), Online and London UK, oct. 2021, abstract PE2/76
Koster K, Saberi P, Fuller SM et al. Pharmacist-Delivered PrEP/PEP acceptability Study. (PDF) Pharmacist-Delivered PrEP/PEP Acceptability Study Northern California Policy Center's Rapid Assessment Project (researchgate.net)
Mayer KH, Molina JM, Thompson MA, et al. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet. 2020 Jul 25;396(10246):239-254. doi: 10.1016/S0140-6736(20)31065-5. PMID: 32711800.
Mugwanya KK, Baeten JM. Safety of oral tenofovir disoproxil fumarate-based pre-exposure prophylaxis for HIV prevention, Expert Opinion on Drug Safety 2016; 15:2, 265-273, DOI: 10.1517/14740338.2016.1128412
Patterson KB, Prince HA, Kraft E, Jenkins AJ, Shaheen NJ, Rooney JF, Cohen MS, Kashuba AD. Penetration of tenofovir and emtricitabine in mucosal tissues: implications for prevention of HIV-1 transmission. Sci Transl Med. 2011 Dec 7; 3(112):112re4)
Ruane P et al. Phase 3 randomized, controlled DISCOVER study of daily emtricitabine/tenofovir alafenamide (F/TAF) or emtricitabine/tenofovir disoproxil fumarate (F/TDF) for HIV pre-exposure prophylaxis: week 96 results. 17th European AIDS Conference, Basel, poster presentation PE3.16, 2019.
Saag MS, Gandhi RT, Hoy JF, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2020 recommendations of the International Antiviral Society-USA Panel. JAMA. 2020;324(16):1651-1669
Zhao A, Dangerfield DT 2nd, Nunn A, et al. Pharmacy-Based Interventions to Increase Use of HIV Pre-exposure Prophylaxis in the United States: A Scoping Review [published online ahead of print, 2021 Oct 20]. AIDS Behav. 2021;1-16. doi:10.1007/s10461-021-03494-4